In the complex field of pediatric urology, few conditions are as common yet as misunderstood as distal hypospadias. Affecting approximately one in every 150 to 300 live male births, it stands as one of the most frequent congenital anomalies encountered by clinicians today. While the diagnosis can be a source of significant anxiety for new parents, modern medical advancements have transformed the treatment landscape. Today, the journey from diagnosis to resolution is characterized by high success rates, refined surgical techniques, and a holistic focus on the child’s long-term physical and psychological well-being.
Defining the Condition: What is Distal Hypospadias?
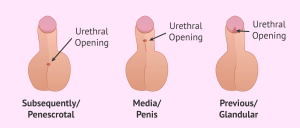
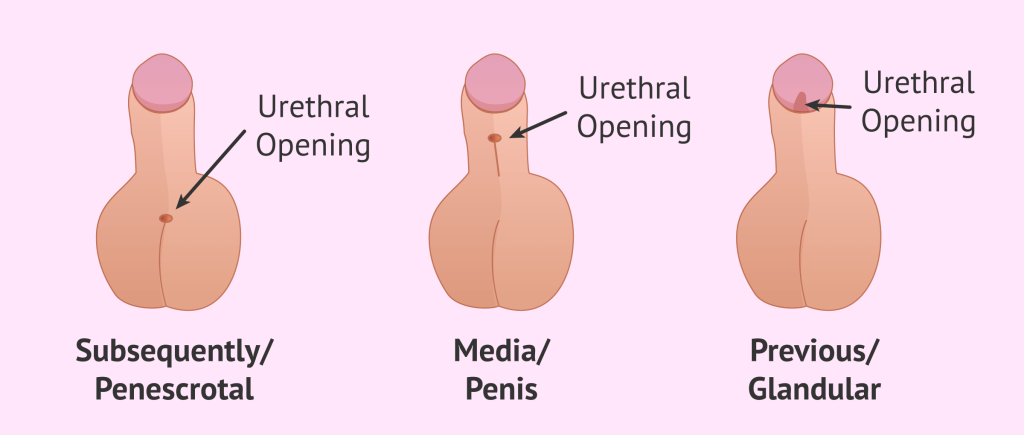
Hypospadias is a developmental condition where the urethral opening-the meatus-is not located at the tip of the penis. Instead, the urethra develops abnormally, exiting on the underside of the shaft. The term distal hypospadias refers specifically to cases where the opening is located near the head of the penis, either on the glans itself or just below it.
Anatomical Markers and Severity
To understand the “distal” classification, one must look at the geography of the condition. In pediatric urology, cases are categorized based on where the urethra ends:
- Distal: The opening is near the tip (glans, coronal, or subcoronal).
- Midshaft: The opening is located along the middle of the penile shaft.
- Proximal: The opening is near the base of the penis or the scrotum.
Distal cases are the most common and generally the least severe. However, even “mild” cases often involve associated features such as a “hooded” foreskin, where the skin does not wrap entirely around the glans, or chordee, a downward curvature of the penis that is most evident during an erection. Understanding these anatomical nuances is the first step for parents in navigating the road to correction.
Etiology: The Interplay of Genetics and Environment
Why does distal hypospadias occur? While science has not yet pinpointed a single “smoking gun,” the consensus among researchers is that the condition is multifactorial, resulting from a delicate interplay between a child’s genetic blueprint and the environment of the womb.
The Genetic Component
Heredity plays an undeniable role. Studies show that if a father has hypospadias, there is an approximate 8% to 10% chance his son will be born with the condition. If a family already has one son with the condition, the risk for the second son rises to about 14%. Geneticists have identified specific variations in androgen receptor genes-the receptors responsible for processing testosterone-that can disrupt the fusion of the urethral folds during the first trimester of pregnancy.
Environmental and Maternal Influences
The development of the male genitalia is a hormone dependent process. Anything that interferes with the endocrine system during the critical window of gestation can potentially lead to distal hypospadias.
- Endocrine Disruptors: Increasing attention is being paid to maternal exposure to “phthalates” found in plastics and certain pesticides, which can mimic or block hormones.
- Maternal Health: Factors such as maternal obesity, diabetes, and even advanced maternal age have been statistically linked to a higher incidence of hypospadias.
- Fertility Treatments: Some studies suggest a slight increase in risk associated with specific assisted reproductive technologies, likely due to the hormonal environment required to sustain the pregnancy.
The Road to Diagnosis: From Birth to Specialist
For most families, the journey begins in the delivery room. A newborn’s first physical examination usually identifies the misplaced urethral opening.
The Initial Assessment
A pediatrician will evaluate the “triple threat” of hypospadias symptoms: the location of the meatus, the presence of chordee, and the configuration of the foreskin. At this stage, a crucial piece of advice for parents is to delay circumcision. The foreskin is often a vital source of “spare parts” (tissue grafts) that the surgeon may need to reconstruct the urethra during the repair process.
Specialist Consultation
Once a diagnosis is suspected, a referral to a pediatric urologist is essential. These specialists use refined diagnostic tools to ensure there are no hidden issues. In some cases, an ultrasound of the kidneys or a voiding cystourethrogram (VCUG) may be ordered to ensure the rest of the urinary tract is functioning correctly. However, for the majority of children with distal hypospadias, the issue is isolated to the exterior anatomy.
Surgical Intervention: Restoring Form and Function
The primary goal of treating distal hypospadias is to create a functional, straight penis with a urethral opening as close to the tip as possible. This allows for a normal urinary stream while standing and prevents future difficulties with sexual function.
Timing is Key
Most pediatric urologists recommend performing surgery when the child is between 6 and 18 months old. At this age, the child is young enough to have no memory of the procedure, but the anatomy is developed enough for precise surgical work. Early intervention also ensures that the repair is complete before the child reaches the age of “potty training” and body awareness.
Modern Techniques: The Snodgrass Procedure
The most common technique for distal repair is the TIP (Tubularized Incised Plate) urethroplasty, often called the Snodgrass procedure. In this operation, the surgeon creates a new urethral tube by incising and rolling the existing tissue. Because it uses the child’s own tissue, the new urethra grows as the child grows.
- Single Stage: Most distal repairs are completed in one surgery lasting roughly 90 to 120 minutes.
- Cosmetic Refinement: Beyond the functional repair, surgeons perform a “glansplasty” to ensure the head of the penis looks as natural as possible.
Post-Operative Care and Recovery
The success of a distal hypospadias repair depends as much on the healing process as it does on the surgeon’s skill. Parents play a lead role in this phase.
Managing the Stent
Following surgery, a small tube called a stent or catheter is often left in the new urethra for 7 to 10 days. This keeps the new channel open while the tissues heal and ensures that urine does not put pressure on the fresh sutures. Modern “double diapering” techniques-where the stent drains into an outer diaper while the inner diaper catches stool-have made this much more manageable for parents.
Monitoring for Complications
While complications are rare in distal cases, parents should be vigilant for:
- Fistulas: A small “leak” or hole that develops along the new urethra.
- Meatal Stenosis: A narrowing of the new opening that makes the urinary stream thin or forceful.
- Infection: Redness or discharge that requires antibiotics.
Long-Term Outcomes: Looking Toward Adulthood
The prognosis for children born with distal hypospadias is overwhelmingly positive. With successful surgical correction, the vast majority of boys grow up to have normal urinary function and a typical aesthetic appearance.
Psychological and Social Development
Research into the long term outcomes of hypospadias repair shows that early, successful surgery prevents the psychological distress that can be associated with “different” anatomy during adolescence. As these boys reach puberty, they generally report levels of sexual function and self esteem that are indistinguishable from their peers.
The Importance of Follow-Up
Even after a successful toddlerhood surgery, it is prudent to have a follow up visit as the child enters puberty. This ensures that the repair has grown proportionately with the adolescent’s body and that the “arc” of the urinary stream remains normal.
Conclusion: Empowering Families Through Knowledge
A diagnosis of distal hypospadias can feel overwhelming, but it is a highly treatable condition with a clear path to resolution. By understanding the anatomical nature of the condition, the importance of surgical timing, and the nuances of post-operative care, parents can move from a place of worry to a place of proactive advocacy.
Working with a dedicated multidisciplinary team-including pediatricians, urologists, and supportive nursing staff-ensures that the child receives not only the best clinical care but also the emotional support needed to thrive. In the hands of modern medicine, distal hypospadias is not a limitation; it is simply a hurdle that, once cleared, allows a child to pursue a healthy and confident future.